Get Easy Health Digest™ in your inbox and don’t miss a thing when you subscribe today. Plus, get the free bonus report, Mother Nature’s Tips, Tricks and Remedies for Cholesterol, Blood Pressure & Blood Sugar as my way of saying welcome to the community!
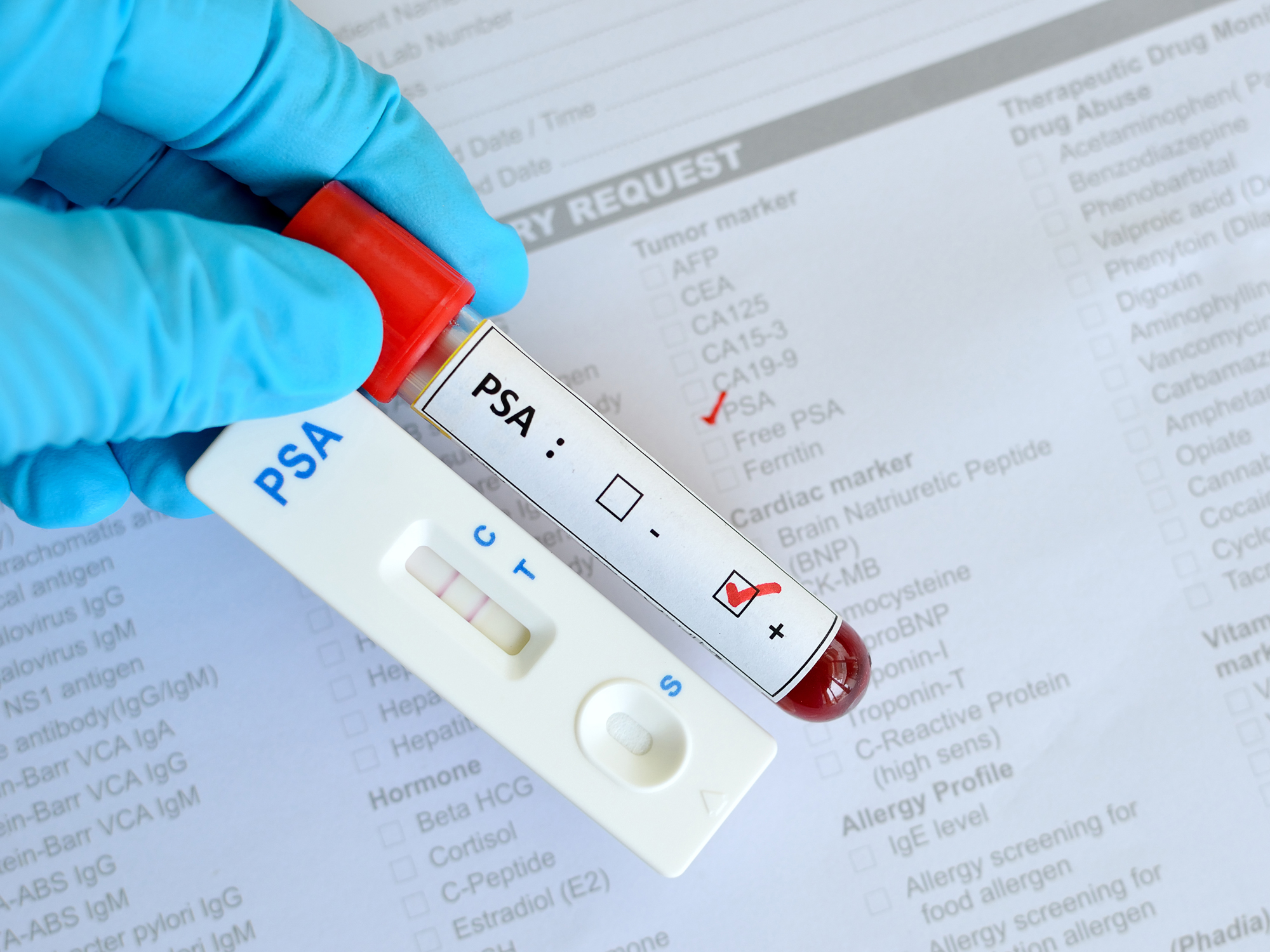
Why a PSA test is still a vital first step
It’s no wonder men are confused…
Over the past few years, various different medical organizations and professionals have changed their minds and recommendations about if and when men should get a PSA (prostate specific antigen) test.
This seeming indecisiveness has left men asking, “Should I get a PSA test for prostate cancer screening, or just blow it off?”
Into this scenario steps again the US Preventive Services Task Force which formerly (in 2012) stated that the PSA test “has no net benefit or that the harms outweigh the benefits.” Now, five years later, the Task Force has issued new guidelines, stating that the test may provide a “small advantage for some men.” It also notes that doctors should “offer or provide this service for selected patients depending on individual circumstances.” Men older than 70, says the Task Force, don’t need to be screened with PSA.
The new guidelines recommend that doctors talk with selected patients aged 55 to 69, and make a prostate cancer screening decision based on their individual and unique needs. Is this responsible? It’s basically saying that your doctor shouldn’t discuss prostate cancer screening you until you’re 55 unless you are in a “high risk group”.
One statistic you should keep in mind is that up to three quarters of men who get the test done are handed a false positive result, which can then lead to unnecessary anxiety, a prostate biopsy, and the risk of side effects from the biopsy.
Also, there are more than a dozen reasons why a PSA level may be elevated, and many have nothing to do with the prostate at all — or more specifically, prostate cancer. Therefore, if you have one elevated PSA value you should probably wait a few weeks and have another test done to see if the results are the same — and not base any immediate action of a single test. In the meantime, you also should consider all of the other factors that can elevate PSA and determine if any of them fit your situation, and if you can do anything to influence a lower PSA value on the next test. For example, don’t ride a bike the morning of the test or have sex, or do other things that may impact the test result.
The bottom line is that the PSA test as part of prostate cancer screening is not foolproof. It definitely has problems.
But the problem with the test is not the test itself but what happens AFTER the test. This is where the USPTF recommendation fails.
Too often doctors “rush to biopsy” for both insurance and liability reasons, rather than adopt a short term “wait and see” to determine if the test result is just an aberration. This is what the USPTF seems to be mostly concerned about — rather than proposing a recommendation and process that actually helps the patient — and actually relieves any anxiety about whether you have a more serious disorder.
Two underlying factors seem to be guiding the USPTF. Firstly, the unnecessary stress that the PSA test sometimes causes. And second, the rush to aggressively treat something that may be benign, slow growing, and cause no immediate harm compared to the side effects of more aggressive treatment. Two valid points.
What’s the solution? I don’t believe it’s to publicly undermine the PSA and its screening benefits like the USPTF is doing with this new recommendation. The problem is in the traditional medical process that follows an “above normal” PSA (usually the “rush to biopsy) — not the PSA test itself.
The PSA test is an indication that “something” is the matter. It may be a number of things unrelated to prostate cancers, but it’s a warning sign — and a call to action (of some sort).
I have many men call or email me every week for advice on prostate and men’s health. Now I’m not a doctor. And I don’t have any formal training in medicine or naturopathy. But I’ve spent the last 10 years running this site and have spoken to hundreds of patients and debated the same amount of doctors over treatments and procedures for prostate cancer. I also have some of the best urologists and medical professionals on my advisory panel.
Why am I so passionate about this? Because I was “that guy” that 10 years ago was thrown into the traditional medical funnel of multiple prostate biopsies and invasive treatments because I had an “above normal” PSA. Now, 10 years on, I still have a PSA of ~4.5-5 but I am cancer free with no indications. Most urologists would want to biopsy me every six months but that’s not going to happen!
But what did my PSA test show me? That “something” was wrong: and that forced me to address the underlying causes of inflammation and other factors that may have been causing my PSA to be higher than normal. At the time I knew nothing about my screening options but I do now. For example, I know there are more accurate tests that are better than PSA for determining prostate cancer. The last time I had my PSA test (3 months ago) I followed it up with a PCA3 urine test after my results again came back high. If the PCA3 had come back positive for cancer cells (it didn’t thankfully) I was slated to have an mpMRI as the next step — a non-invasive procedure that uses powerful imaging to detect cancer cells. If the mpMRI had come back showing something suspicious only then would I have had a prostate biopsy — as only a biopsy can determine the stage and grade of cancer if identified — and provide “some” of the information needed to determine the course of treatment going forward (if any).
I’m lucky to be under the care of one of the top urologists in the US who is also the Medical Director of the Prostate Cancer Foundation. Dr. Stu Holden is at the cutting edge of treatment options and the use of non-invasive screening options for prostate cancer. I’m also privileged to have Dr. Dan Sperling on our Experts Panel who is leading efforts in focal treatment of prostate cancer and mpMRI imaging for prostate cancer detection. These doctors are leading the way in new screening and monitoring procedures for prostate cancer that are less invasive and provide more accurate detection of prostate cancer.
But the detection process still starts with the PSA test, and for many reasons it will continue like this for some time. So to publicly undermine the importance of the test in the media like the USPTF is doing is irresponsible and gives men more of a reason to avoid the dreaded “digital rectal examination” and ignore the need for a PSA test at all.
So back to my earlier point… When I’m asked about what to do after a high PSA reading, what do I say?
- That I’m not a doctor and you need to talk to your urologist about your options.
- But you might want to wait, and test again.
- Look at other options after a high reading such as a PCA3 urine test or one of the other alternatives to the PSA test.
- If the PCA3 is positive then look to get an mpMRI.
- And only after all that, and armed with more accurate test results, discuss the next steps with your urologist including all your treatment options or whether to just do nothing at all.
Again, I’m not a doctor. But I’m someone who knows more than 99% of the population about this. My advice? Read as much as you can and ask your urologist about alternatives to having a biopsy if he/she wants to immediately move to that next step after a high PSA test. Just don’t use the USPTF recommendations as an excuse to avoid getting tested at all.
Remember, prostate cancer is a serious disease. The decisions you take about your treatment and screening options will determine your life and lifestyle going forward. Don’t avoid the PSA test. I started getting tested at 38. More and more men are getting prostate cancer in their 30’s and it’s not just an “old man’s disease.” Taking responsibility for your health starts with knowing your test results.
Treat the PSA test like you would a blood pressure or cholesterol test. Knowing something is not normal gives you the power to take action for better health in the long term.
Sources:
-
Prostate Cancer Screening Draft Recommendations — United States Preventive Services Task Force
-
Prostate-Specific Antigen (PSA) Test — National Cancer Institute












