Get Easy Health Digest™ in your inbox and don’t miss a thing when you subscribe today. Plus, get the free bonus report, Mother Nature’s Tips, Tricks and Remedies for Cholesterol, Blood Pressure & Blood Sugar as my way of saying welcome to the community!
Insulin resistance: What you need to know
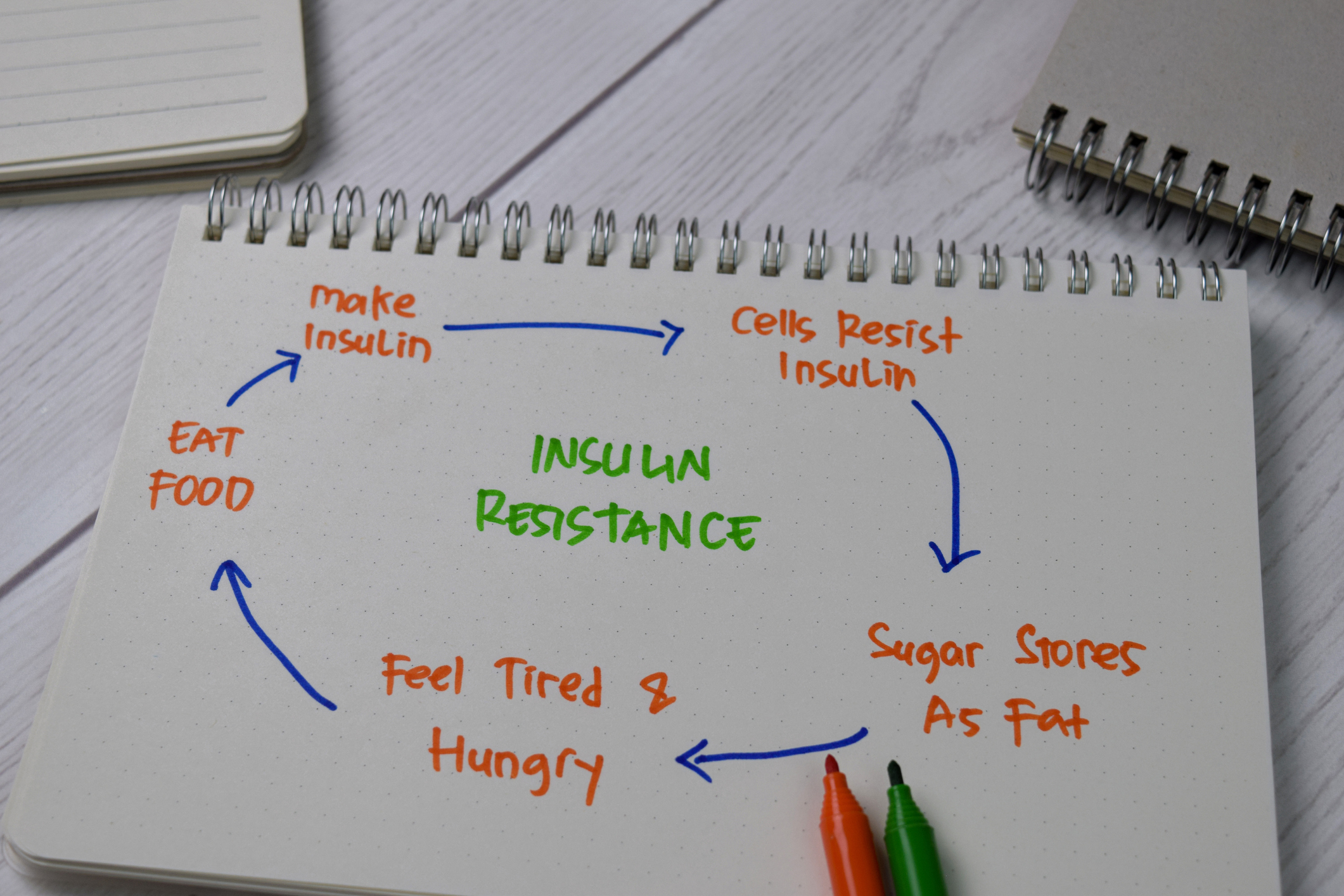
Type 2 diabetes, pre-diabetes, insulin resistance. They’re all manifestations of the same metabolic dysfunction, just to a different degree. And all individuals who develop type 2 diabetes are initially pre-diabetic. And all pre-diabetics are initially insulin resistant.
So how does insulin resistance develop?
Through consuming excess calories and, especially, excess fat.
Our bodies are incredibly efficient energy storage machines. We are evolutionarily pre-designed to always be prepping for surviving lean times.
This may have been exceedingly useful when we lived on the savannah and faced periods of starvation. It’s far less helpful when we’re surrounded by food everywhere we go. In fact, it can be downright counterproductive.
Here’s what happens…
How it begins
When we consume fats, they get broken down into triglycerides in the digestive system and are then absorbed. Triglycerides are also formed inside our bodies when we consume excess calories.
Triglycerides are sources of concentrated energy. And regardless of whether they’re absorbed or formed internally, they end up circulating through our bloodstreams and then get stored in three main places — in adipose tissue (fat cells), in muscles and in the liver.
Fat cells are designed for fat storage and can accept as many triglycerides as we throw at them. Liver and muscle? They also accept triglycerides readily, but at some point, they start to rebel. After all, liver and muscle cells have much more to get done in a day than just store energy!
Turns out, it’s hard to stop triglycerides from getting into liver and muscle cells for excess energy storage. So the body pursues an alternative strategy and starts to blunt cellular entry of other forms of energy. What’s another form of energy? Glucose.
Normal cells listen to insulin when it comes knocking to ask for a glucose molecule to enter. Triglyceride-laden cells become progressively hard of hearing and need insulin to knock louder and louder to respond. In other words, they become resistant to the requests that insulin makes. The body’s response? Make more insulin so it knocks harder! The cellular response? Become progressively even more hard of hearing.
The hidden dysfunction
And this manifests in a predictable blood sugar profile decline. Initially, the dysfunctional metabolism is hidden by more and more insulin being pumped out by the pancreas. Your blood sugar level might be normal, but you need way more insulin to get it into a normal range. At this point, you are insulin resistant.
Eventually, the pancreas can’t make enough insulin to knock as loud as it needs to, and blood sugar levels start to rise. At this point you are pre-diabetic.
Finally, the pancreas gets tired, can’t keep up and gives up — eventually pumping out less and less insulin — and voila! You’re a type 2 diabetic.
A few things that should become obvious to you:
- Pre-diabetes is a giant misnomer because it’s not a pre-disease! It’s a sign that your metabolism is a LONG way from normal.
- Waiting for diabetes to develop before you take your blood sugar levels seriously is a highly flawed strategy. The sooner you start an all-out effort to get your metabolism right, the better. Don’t wait until your pancreas is exhausted!
- A high-fat diet, especially the ketogenic approaches that are in vogue for diabetic patients these days, might not be such a good idea. After all, a high-fat diet directly contributes to triglyceride stores. The reason ketogenic diets “work” is because they limit carbs, meaning it doesn’t matter if your cells remain deaf to insulin! There’s nothing to knock about: blood sugar levels may improve — but this belies the underlying dysfunctional metabolism which stays unchanged.
Editor’s note: Are you feeling unusually tired? You may think this is normal aging, but the problem could be your master hormone. When it’s not working, your risk of age-related diseases skyrockets. To reset what many call “the trigger for all disease” and live better, longer, click here to discover The Insulin Factor: How to Repair Your Body’s Master Controller and Conquer Chronic Disease!













