Get Easy Health Digest™ in your inbox and don’t miss a thing when you subscribe today. Plus, get the free bonus report, Mother Nature’s Tips, Tricks and Remedies for Cholesterol, Blood Pressure & Blood Sugar as my way of saying welcome to the community!
What they left out of the latest cholesterol guidelines that you need to know
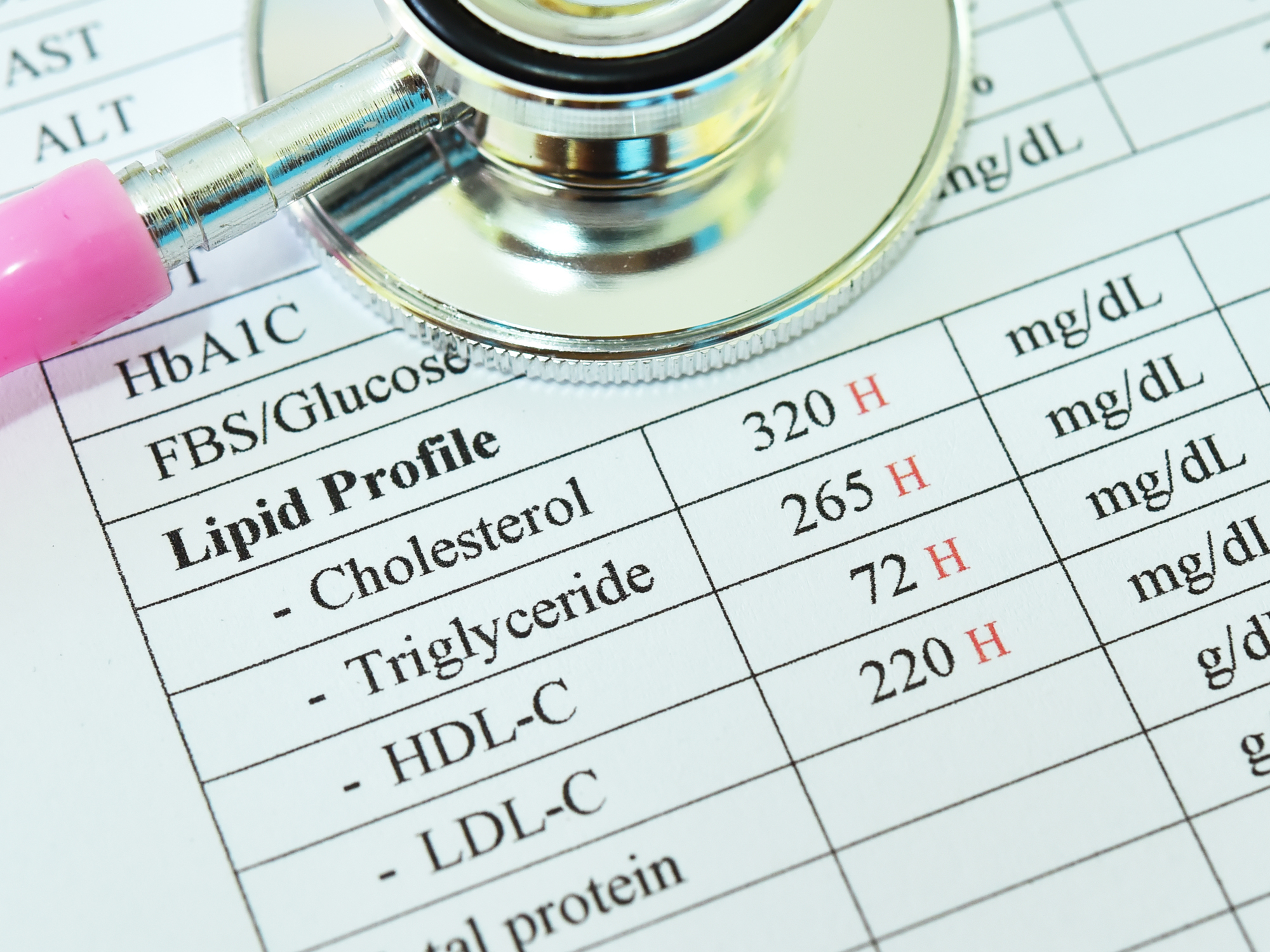
The newest cholesterol guidelines that were presented at the American Heart Association conference leave much to be desired…
Namely, the absence of specific, detailed instructions on how to help patients succeed at the hardest part of their treatment plan — nutrition.
However, the guidelines do allow for a more “personalized” approach to drug therapy — which could allow some patients to REDUCE the number of drugs they are taking (a good thing), though some will end up on MORE (not so great).
That’s because the latest guidelines are much more focused on helping manage risk and sorting patients more precisely into lower and higher risk groups – as well as providing much more latitude in terms of how much medication to use to get patients to goal.
If your doctor isn’t revisiting how he’s treating your cholesterol, you should ask him about it, after you see what’s new…
Here’s what’s new (and better) for cholesterol management
1. The new guidelines go back to measuring cholesterol numbers. I know this sounds crazy, but the previous document instructed physicians to just pick out people who should be on statins (about 70 million Americans), and then just put them on the maximum tolerated dose of statin drugs. No follow-up labs required.
Turns out — not unexpectedly — that as a result, some patients were over-medicated while others were under-treated. Apparently, numbers DO matter, and it makes sense to achieve specific cholesterol goals to minimize risk.
Why is this good? It now permits physicians to use the LOWEST possible medication dose to achieve a desired cholesterol result.
2. The new guidelines encourage the use of other medications in addition to statins in people who are not at goal LDL levels. The old guidelines relied on statins alone. Now drugs like ezetimibe (Zetia®), bile acid sequestrants (like Welchol® and Questran®) and PCSK9 inhibitors (like Repatha®) are to be considered as adjunctive therapy if cholesterol goals are not achieved with statins alone.
Why is this good? It provides additional options to attain lower cholesterol levels in high-risk patients who can’t get there on statins alone.
3. The new guidelines acknowledge that individuals may bring additional risk factors to the table that tip the scale towards starting medications.
FINALLY risk factors such as family history of heart disease, elevated lipoprotein A, elevated apoprotein B, metabolic syndrome, premature menopause, chronic kidney disease and inflammatory disorders (like rheumatoid arthritis) – all of which are KNOWN to be associated with a more accelerated atherosclerotic process – are to be considered when determining if a patient would benefit from starting cholesterol-lowering drugs.
Why is this good? The previous guidelines generally ignored these additional risk considerations, which probably left a lot of people UNDER-treated.
4. The new guidelines encourage the use of coronary artery calcium (CAC) scanning in the situation where the risk/benefit of starting drugs is uncertain. If you don’t know what CAC scanning is, you can find out more information about it here.
Why is this good? A CAC of 0 (zero) indicates that the individual with that score is at an incredibly low risk of experiencing a cardiovascular event in the near term (over the next few years), meaning that adding statins to the mix (though it might make cholesterol numbers look better) will not actually affect their risk or outcome.
Why is this great? It allows some people with even high cholesterol levels to avoid medications (at least temporarily).
Unfortunately, the latest guidelines probably do nothing to reduce the overall number of people who would be candidates for statin drugs. And that underscores how badly we are failing at helping people achieve healthy lifestyles.
Leveraging the most important piece of the puzzle
Although drugs can be a good thing when really necessary and do work, I always come back to the over-riding truth, which is that people who live long well do so because they LIVE WELL.
Not because they’re on the perfect combination of the latest drugs prescribed in accordance with the latest guidelines.
Medications are an ADJUNCT to risk reduction. They are not the core of what we should be doing to achieve healthy longevity (which is the ultimate goal of all therapy). Which is why I continue to see these new Guidelines as only addressing a small portion of what we should be doing.
The full Cholesterol Guidelines document is 120 pages long. How much of the document is formally devoted to diet? One paragraph.
Related: 6 ways to manage cholesterol without drugs or disease risk
You read that right. They practically left out one of the most valuable tools for achieving optimal cholesterol levels.
Even though high cholesterol is driven in whole or in part by what we eat. And even though data shows that people who lower their cholesterol with drugs alone — and don’t pay attention to the diet bit — may not benefit much from the LDL lowering they achieve.
And let’s not forget that dependence on medication has its drawbacks, including the well-reported negative side effects of statin use.
So here are some hints on how to leverage the best parts about the new guidelines and help yourself with food:
- To attain the lowest possible medication dose to achieve your cholesterol goal, eat in a way that supports cholesterol lowering. Even if your diet doesn’t budge the numbers much, know that it is budging your RISK.
- Before using additional medications to achieve a cholesterol goal when you can’t get there with statins alone, try structured dietary change as the first next step. And then measure your cholesterol to check the effect of your nutrition efforts. The Guidelines encourage other drugs, but nothing says you can’t try food first.
- If you have risk factors that put you at a special disadvantage when it comes to developing atherosclerosis, be extra vigilant about what you eat.
- If you have a 0 CAC score, eat in a way that will help you keep that low score. So that when you’re tested again in 3-5 years, you can get another reprieve from medications.
When it comes to diet, I always encourage everyone to do as much as they can on their own.
But I also know that it’s not always easy to stay on track or even know what to do. Which is why Step One Foods exists — to help support all your efforts to reduce your dependence on medications, to reduce your risk and to live longer, well.













