Get Easy Health Digest™ in your inbox and don’t miss a thing when you subscribe today. Plus, get the free bonus report, Mother Nature’s Tips, Tricks and Remedies for Cholesterol, Blood Pressure & Blood Sugar as my way of saying welcome to the community!
Stents don’t work
That was the conclusion of a study that recently rocked the cardiology community.
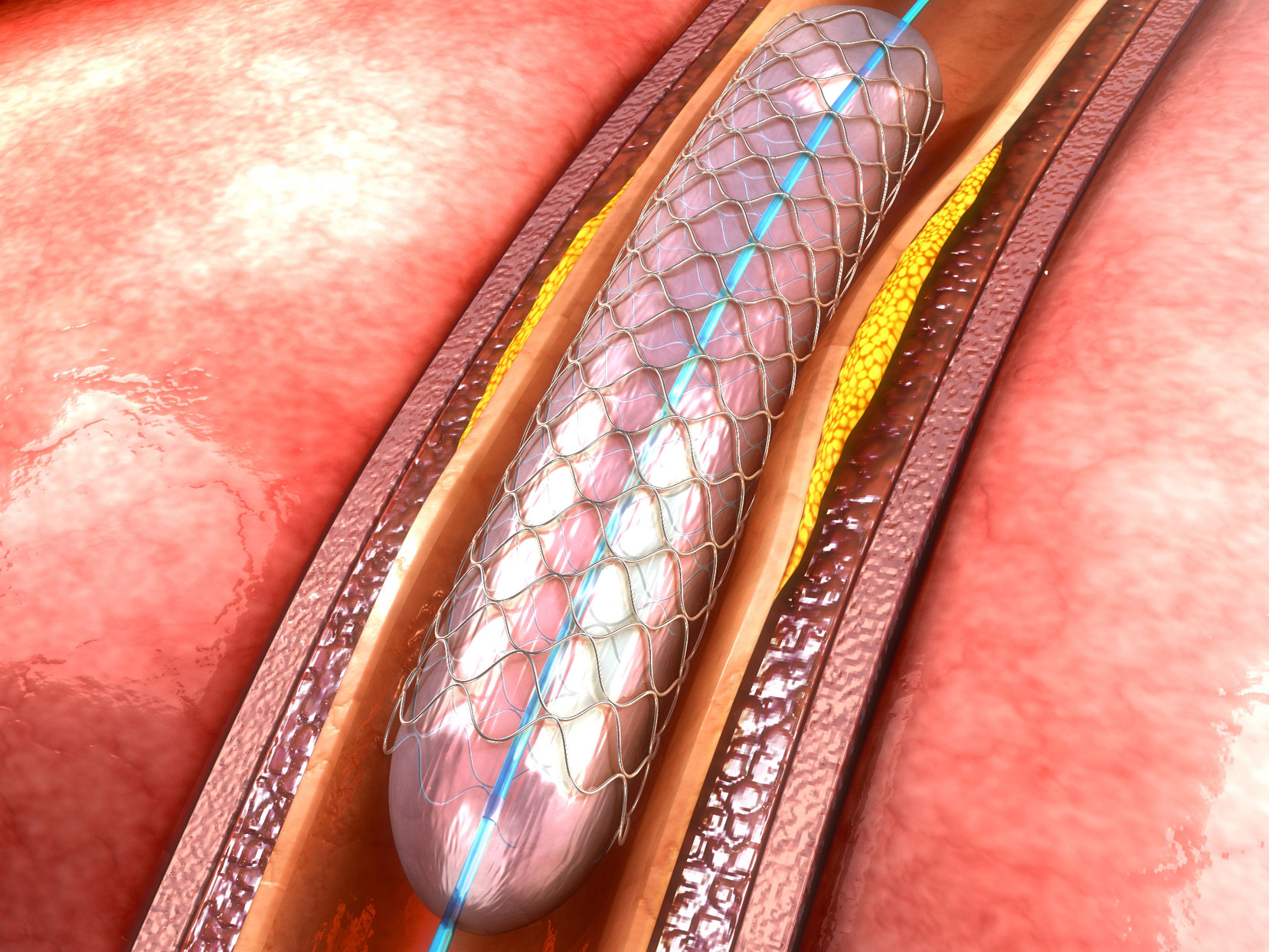
Stents have been used to open blocked heart arteries for decades. The first one was implanted in 1986 and the use of stents quickly became commonplace.
That’s because the little mesh devices, when expanded within arteries, are really good at keeping those arteries open.
Inserting a stent costs between $11,000 and $41,000, and it’s estimated that at least 500,000 people undergo the procedure each year.
There is no question that stents can be lifesaving when they’re part of the treatment protocol for a heart attack. But most stents are not put in during heart attacks.
Most stents are implanted because a blockage has been discovered after someone has been evaluated for angina (chest pain that occurs with exertion).
And that’s where things get fuzzy…
Stenting’s not all it’s chalked up to be
At first, everyone — patients and doctors alike — were convinced that inserting stents in people with angina prevented future heart attacks. Turns out that’s not the case…
A large study, called the COURAGE trial, published 10 years ago, found that there was no difference in the rates of subsequent heart attack, death or stroke between patients treated with stents as compared to those treated with medications alone.
But stents kept getting implanted — lots of them. Because everyone — patients and doctors alike — were convinced that stents were really good at eliminating angina. Turns out that’s not the case either.
A new study — the one that rocked the cardiology universe — found NO DIFFERENCE in chest pain relief among patients treated with stents compared to those undergoing a sham procedure.
The study was done in England and all patients were given drugs to reduce the risk of heart attack and prevent blood clots. Neither the patients nor the clinicians observing them during 6 weeks of post-procedure follow-up knew who got a stent and who didn’t.
And here’s the huge surprise finding — after 6 weeks, patients reported improvement in angina symptoms and demonstrated improved stress test results, regardless of whether they received a stent or not.
The chance that this one study will change practice patterns is low. Already, questions are arising as to whether 6 weeks of follow-up is enough.
But the findings should truly give us pause as to how we treat heart disease today. Because pre-conceived notions about the effectiveness of our standard therapies just might be completely wrong.
What isn’t in dispute?
- A stent can save your life if you’re in the throes of a heart attack.
- Lifestyle change — and especially a better diet — can reverse blockages, improve blood flow and help you avoid that heart attack in the first place.
A less invasive ‘treatment’
Regarding number two, especially a better diet… this is where most patients have been let down by the people they look to for health advice.
Not only are there perverse incentives that steer physicians to prescribe drugs instead of food, but as a medical doctor I can attest firsthand we’re not taught to.
As a Mayo Clinic and John Hopkins trained cardiologist, I completed over 80,000 hours of instruction to become a physician.
Those 80,000 hours included everything from learning the basics about anatomy and physiology to determining which test, drug and procedure to use for almost any condition. Medical school and cardiology residency also taught me everything I needed to know to treat all sorts of heart problems, no matter how big or small.
But I was never taught about nutrition — the factor that’s causing all the heart disease in the first place.
Here’s a fact: Food can be just as powerful as medicine in treating many health problems.
In fact, medical literature is actually voluminous and consistent about what nutrients in what amounts impact cholesterol levels and heart health — namely 10 grams of whole food fiber, 3 grams of ALA omega-3 fatty acids, 2 grams of plant sterols, and 5000 µmoL antioxidants per day.
The problem is that we live in a world where it’s almost impossible to support health through food. And isn’t that a tragedy?
For more on real food, real science, and real results, read more at steponefoods.com.
Sources:
- Optimal Medical Therapy with or without PCI for Stable Coronary Disease — The New England Journal of Medicine
- Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial — The Lancet
- ‘Unbelievable’: Heart Stents Fail to Ease Chest Pain — The New York Times













