Get Easy Health Digest™ in your inbox and don’t miss a thing when you subscribe today. Plus, get the free bonus report, Mother Nature’s Tips, Tricks and Remedies for Cholesterol, Blood Pressure & Blood Sugar as my way of saying welcome to the community!
What you should know about peripheral artery disease
Peripheral artery disease affects about 8.5 million Americans.
Gone undetected and untreated, peripheral artery disease can be life-threatening. It can lead to stroke, heart attack, and limb amputations.
Yet many people don’t even know they have peripheral artery disease. Are you one of them?
What is peripheral artery disease?
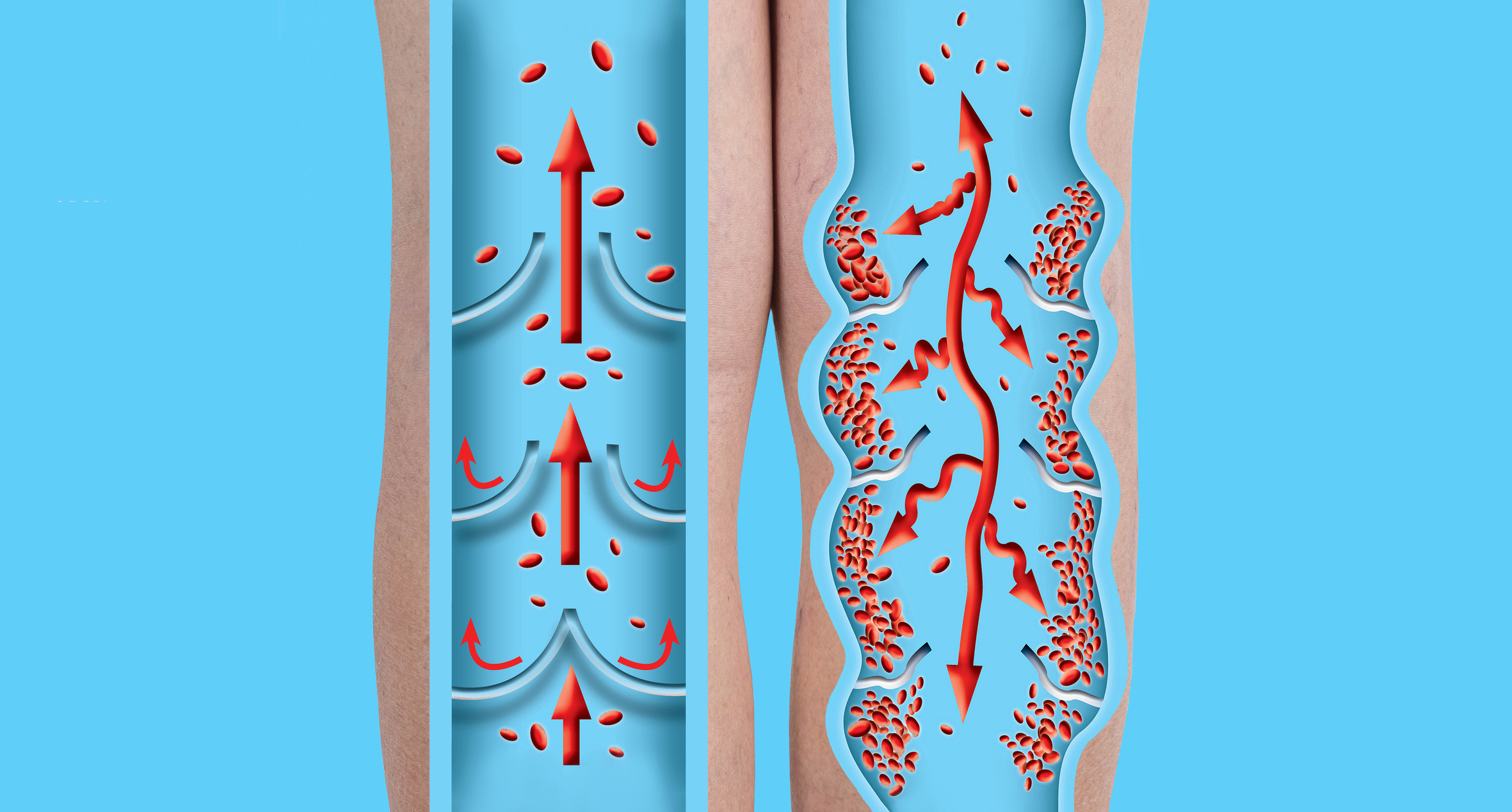
Peripheral artery disease, or PAD, is similar to coronary artery disease. Both involve a buildup of plaque inside the arteries, which slows the flow of blood that nourishes all parts of the body and increases risk of clots.
But while coronary artery disease involves the arteries leading directly out of the heart, PAD involves arteries that carry blood to your extremities, most often the legs.
Left undiscovered and untreated, this reduced blood flow to the legs and feet can cause heart attack, stroke, kidney problems, and gangrene in the foot, resulting in amputation.
What are the symptoms of PAD?
The most common symptom of PAD is leg pain or cramps when you walk. This is known as claudication (pain caused by too little blood flow to muscles during exercise).
With claudication, your legs may also feel heavy, numb, weak or tired. These symptoms will ease once you stop exercising.
The problem, though, is that you may have no symptoms at all, or very mild ones until your arteries are more than halfway narrowed by plaque.
As this condition worsens, you may feel pain or burning in your feet, even when you are at rest. The skin on your feet may feel cool, look shiny, or change colors. You may also develop sores on your feet that don’t heal.
Another problem is that tired, heavy legs are easy to write off as arthritis, or just part of getting older. That’s why PAD often goes undiagnosed until symptoms become severe.
How is PAD diagnosed?
If you are experiencing even mild leg pain or cramps on a consistent basis, you can ask your doctor to do an ultrasound to see if there are narrowed or blocked arteries in your legs.
With a physical exam, your doctor can also use a cuff to obtain an ankle-brachial index, or ABI. This compares the blood pressure in your leg with that in your arm and helps determine whether arteries in the leg are narrowed or blocked.
Angiography is a more invasive test where dye is injected into your arteries through a catheter tube. Doctors then use special X-rays or CT scans to scan and track your blood flow.
Treatment for PAD
Once you are diagnosed with PAD, your doctor will prescribe medications both to ease symptoms and to keep the condition from advancing.
Medications to lower cholesterol and blood pressure are often the first line of treatment. You may also be prescribed a daily aspirin or a drug known as clopidogrel (Plavix) to prevent blood clots and improve blood flow.
To ease leg pain, your doctor may prescribe cilostazol (Pletal) or pentoxifylline (Pentoxil), drugs that widen narrowed blood vessels and improve blood flow, so that you can walk and exercise with less pain.
If medications don’t help, your doctor may recommend surgery to treat PAD pain. There are several options.
Angioplasty is the insertion of a tiny balloon that’s inflated to widen the arteries. A tube called a stent can also be placed to hold open these vessels. Your doctor can also remove blockages or inject a drug to dissolve blood clots.
Preventing and managing PAD
There are risk factors for PAD that you cannot control but should be aware of. These include being older than 60, having kidney disease, having a family history of heart disease, and having high levels of the amino acid homocysteine. Also, African Americans have double the risk of PAD compared to people of other races.
The good news, though, is that there are quite a few risk factors you can control.
In 2019, OmegaQuant — an independent, CLIA-certified lab that offers Omega-3 Index testing to researchers, clinicians and the public, and sets the standard for fatty acid testing, found an association between PAD and omega-3 deficiency.
The investigators compared the Omega-3 Index in 145 patients with PAD to 34 controls without PAD and found:
- The Omega-3 Index was significantly lower in the PAD patients than the controls (5 percent vs 6 percent).
- For every 1 percent unit reduction in the Omega-3 Index, the odds of being a PAD patient increased by a whopping 39 percent.
- For every additional pack-year of smoking, the odds of being a PAD case increased by 4 percent.
Not surprisingly, like smoking, other risk factors for PAD are the same as those for heart disease, including metabolic syndrome, obesity, high blood pressure, high cholesterol, and diabetes.
If you smoke, you can get help with quitting. Obesity, high blood pressure, high cholesterol and high blood sugar (in combination, known as metabolic syndrome) can be tackled by changing your diet. The DASH diet is a great place to start. Exercise is important, too.
Editor’s note: Have you heard of EDTA chelation therapy? It was developed originally to remove lead and other contaminants, including heavy metals, from the body. Its uses now run the gamut from varicose veins to circulation. Click here to discover Chelation: Natural Miracle for Protecting Your Heart and Enhancing Your Health!
Sources:
A Visual Guide to PAD — Web MD
About Peripheral Artery Disease (PAD) — American Heart Association
Peripheral Arterial Disease (PAD) — Centers for Disease Control and Prevention (CDC)














